In Anticipation of a Highly Virulent SARS-CoV-2 Variant:
An ADDENDUM
Rob Rennebohm, MD
October 1, 2023

This article represents an extended ADDENDUM to an earlier article entitled: In Anticipation of a Highly Virulent SARS-CoV-2 Variant:
https://notesfromthesocialclinic.org/in-anticipation-of-a-highly-virulent-sars-cov-2-variant/
The purpose of both articles is to provide information that might help the general public, health care professionals, and health departments to optimally prepare for and treat a potential highly virulent SARS-CoV-2 variant.
INTRODUCTION:
In his book, The Inescapable Immune Escape Pandemic, and on his website, Dr. Geert Vanden Bossche (GVB) has explained his scientific analysis of and deep concerns about the COVID-19 mass vaccination campaign. For a summary of his analysis and concerns, see: https://www.voiceforscienceandsolidarity.org/scientific-blog/the-emergence-of-a-highly-virulent-variant-is-inescapable and https://www.trialsitenews.com/a/how-has-the-covid-19-mass-vaccination-campaign-made-the-natural-selection-and-rapid-propagation-of-a-highly-virulent-variant-highly-likely-44952cc7
Dr. Vanden Bossche is deeply concerned that:
• The COVID-19 mass vaccination campaign, which was implemented in the midst of an active pandemic, has placed great sub-optimal1 population-level immune pressure on the SARS-CoV-2 virus.
1Note: An “optimal” vaccine for use during a period of viral exposure (e.g., during a pandemic) is one that induces sterilizing immunity in the vaccinee, such that the virus is killed (i.e., becomes unable to replicate and spread to others) when the vaccinee subsequently encounters the virus. When a sufficiently high percentage of the population develops sterilizing immunity to a particular virus, herd immunity is achieved and the pandemic ends, because the virus runs out of accessible, susceptible new hosts and the transmission and infection rate therefore drop below a minimal threshold required to cause symptomatic infection in the remainder of the population. “Suboptimal” immunization induces immunity that may thwart viral replication and transmission but does not adequately prevent viral replication and transmission, and thereby allows the virus to survive and spread. Use of the COVID-19 vaccines during a pandemic leads to suboptimal immunity—i.e., their use during a pandemic does not result in sterilizing immunity in vaccinees, does not result in killing of the virus, does not prevent infection or transmission, and therefore their use does not contribute to herd immunity. In order for COVID-19 vaccines to contribute to herd immunity when administered during a pandemic, they would need to possess sterilizing capacity, which they do not have. In fact, they interfere with development of herd immunity. At best, COVID-19 vaccination during a pandemic may temporarily reduce disease severity (reduce hospitalizations and death), as will be explained later.
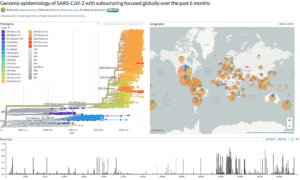
• This suboptimal population-level immune pressure is responsible, predictably, for the natural selection and dominant propagation of a vast array and continuing succession of increasingly infectious new “immune escape” variants—e.g. the many Omicron variants. As the COVID-19 vaccines are directed at spike protein and as spike protein is responsible for viral infectivity, highly vaccinated populations exert immune selection pressure on viral infectiousness. This explains why these newly emerging variants are more and more infectious.
• When individuals received COVID-19 vaccination prior to experiencing productive natural infection with the SARS-CoV-2 virus, their immune status became abnormal, particularly if a mRNA vaccine was used. Specifically, their adaptive immune system has needed to do things it normally has not needed to do (e.g., produce high levels of infection-enhancing but protective virulence-inhibiting PNNAbs2 and substantial levels of SIR3-created broadly neutralizing antibodies); and their cell-based innate immune system has been sidelined, the training of their innate immune system has been compromised, and, therefore, their innate immune system has been unable to adapt to the more infectious environment and has been unable to contribute to the development of sterilizing immunity.
• During the Omicron era, the immune system in vaccinated individuals has made four main adjustments in an effort to protect vaccinees from severe disease: namely, the SIR phenomenon;3 isotype switching of SIR-created antibodies to anti-inflammatory SARS-CoV-2 IgG4 antibodies; production of high levels of virulence-inhibiting PNNAbs;2 and activation of cytolytic T lymphocytes (CTLs). These protective immune adjustments have given the false impression that SARS-CoV-2 variants have become milder, less threatening, and will soon become endemic and relatively harmless. However, these immune adjustments are unstable, unsustainable, will ultimately fail to protect, and are problematic—both at an individual level (e.g., predisposing vaccinees to autoimmunity, malignancy, and compromised control of infections) and at a collective level (contributing to the suboptimal population-level immune pressure that is responsible for the natural selection and dominant propagation of a vast array and continuing succession of increasingly infectious new “immune escape” variants). These adjustments have created a falsely reassuring “calm” before an inevitable “storm.”
• The suboptimal population-level immune pressure will inevitably (and soon) lead to the natural selection and rapid propagation of an immune escape variant (or variants) that is able to overcome the key virulence-inhibiting measure that the immune system of vaccinated individuals has been using to protect vaccinees from severe disease and death—namely, virulence-inhibiting PNNAbs (polyreactive non-neutralizing antibodies).
• Highly virulent SARS-CoV-2 variants will have great potential to cause severe illness and death (the above-mentioned “storm”), particularly in highly (and rapidly) vaccinated countries, especially in vaccinated individuals who did not experience productive natural SARS-CoV-2 infection prior to their vaccination, particularly if vaccinated with mRNA vaccines.
The general public and their physicians have a right to know about GVB’s concerns, analysis, and conclusions so that they can proactively prepare for the highly likely arrival of a potential highly virulent variant. It is in that spirit that the following anticipatory thoughts and suggestions are offered.
2Note: PNNAbs = Polyreactive non-neutralizing antibodies. The virulence-inhibiting effect of PNNAbs is due to the following: There is evidence that inflammation due to acute viral respiratory infection (like SARS-CoV-2 infection) causes the virus to adsorb (instead of internalize) onto (become tethered to) the surface of patrolling migratory dendritic cells (a type of immune cell), which then carry the virus from the upper respiratory tract (URT) down to the lower respiratory tract (LRT) and potentially to other internal organs. Upon arrival in the LRT, these virus-laden dendritic cells may then transfer the tethered virus to epithelial cells in the LRT, thereby infecting those cells, which in turn infect neighboring epithelial cells, resulting in potentially severe LRT infection. This is referred to as “trans-infection” of the LRT.
PNNAbs are able to bind to virus that is tethered to these migratory dendritic cells. When PNNAb is bound to tethered virus, the virus is not easily released from the dendritic cells and cannot easily trans-infect epithelial cells in the LRT. In this way, PNNAbs are “virulence-inhibiting” and thereby protect against severe infection in the LRT and other internal organs (i.e., protect against severe disease and death). The virulence of an anticipated “highly virulent variant” is predicted to be due to the ability of the variant to overcome (become resistant to) the virulence-inhibiting effect (but not the infection-enhancing effect) of the PNNAbs. That is, the PNNAbs will still be able to enhance viral infectiousness while failing to prevent the highly virulent variant from trans-infecting cells in the LRT. Accordingly, “enhancement” of severe disease in the LRT will result.
3Note: SIR = Steric Immune Refocusing. In the context of SARS-CoV-2, SIR refers to the redirection (refocusing) of the immune system to produce neutralizing antibodies against conserved immune-subdominant epitopes of the spike protein when pre-existing poorly neutralizing (out-of-date, no longer effective) antibodies sterically hinder (physically block) immune recognition of the variable immune-dominant epitopes of the spike protein (because, though ineffective, those antibodies, nevertheless, still bind to the immunodominant epitopes). Vaccinated individuals, via the SIR phenomenon, produce broadly reactive cross-neutralizing antibodies to immunosubdominant spike-associated domains. These SIR-created high avidity antibodies have temporarily provided efficient cross-neutralizing activity. These SIR-created antibodies partially compensate for the ineffectiveness of obsolete (out-of-date) vaccine-induced neutralizing antibodies (e.g. the original vaccine-induced neutralizing antibody to the spike protein of the now extinct Wuhan strain of SARS-CoV-2).
A BRIEF REVIEW OF THE USUAL CLINICAL COURSE OF SEVERE COVID-19—AT LEAST UP UNTIL NOW:
To date, the clinical course of severe COVID-19 has typically had two major phases—an initial acute viral phase (typically lasting 7-10 days) followed by a hyperinflammatory phase, which has usually become clinically apparent after day 7 and increases during the second and third weeks of the illness. The hyperinflammatory phase is due to an intense and dysregulated immune reaction to the virus and is characterized by varying degrees of “cytokine storm” and associated inflammation within the lower respiratory tract (LRT) and potentially in other internal organs. Although this hyperinflammatory reaction has potential to contribute to reduction of viral load, it also has potential to cause severe inflammatory damage. By the time the hyperinflammatory phase has reached its peak, the viral load has usually already greatly diminished—thanks primarily to the immune system, plus help from anti-viral therapies and immune system-supportive nutraceuticals, if those therapies are given and are effective—but such diminution of viral load is not guaranteed.
An extreme example of severe COVID-19 would be a combination of an extremely high and undiminishing viral load and an extraordinarily intense and ineffective hyperinflammatory (cytokine storm) reaction that is doing severe damage (e.g., causing damage to multiple organs).
Fortunately, to date, most people who have developed COVID-19 have not developed severe COVID-19. Instead, they have experienced only an acute viral phase (without a clinically apparent hyperinflammatory phase), or they have developed only a mild to moderate hyperinflammatory phase, at most. They have been able to eliminate the virus (or at least greatly diminish the viral load) within 7-10 days, and they have ultimately had a good outcome.
To date, most patients with severe COVID-19 who have ended up in the ICU (typically during the second or third weeks of the illness) and have died from their COVID-19 have done so primarily because of an extraordinarily severe and damaging hyperinflammatory phase (with severe cytokine storm and associated immune-mediated lung disease). In such patients, secondary bacterial infection of the lungs can be a complicating factor, as can abnormal thrombosis (clotting).
ANTICIPATORY QUESTIONS:
In anticipation of the possibility that variants displaying a high level of virulence in highly vaccinated populations may emerge and rapidly propagate, several questions need to be proactively raised and addressed, now:
• When/if a potentially highly virulent variant arrives, who will be most affected, who will be least affected, and why?
• How will the illness it causes behave? What is the spectrum of possibilities?
• How severe will the illness be?
• How quickly (after onset of symptoms) will peak severity of illness occur?
• How overwhelming will the acute viral phase be and how long will the acute viral phase last?
• In what percentage of patients will there be a hyperinflammatory phase (e.g., “cytokine storm”): to what extent will a highly susceptible person have time, opportunity, and wherewithal to even mount a cytokine storm? If able to mount a cytokine storm, how severe will it be; how soon will it occur after onset of symptoms; to what extent will it reduce viral load (i.e. be helpful); to what extent will it be harmful (e.g., cause life-threatening organ damage)
• How effectively will the human immune system be able to respond to a highly virulent variant?
• Will the efficacy of the immune response and the severity of illness depend on vaccination status?
• How can the clinical course of the illness be best monitored and interpreted?
• What are the indications for early introduction of anti-viral therapy for a virulent variant? What other early treatments may be helpful?
• What anti-viral therapy has the most favorable benefit/risk ratio?
• How is the hyperinflammatory phase/”cytokine storm” recognized and best managed?
• How is the threat of COVID-19-related thrombosis best managed?
• What is the role of home use of pulse oximetry?
• How can COVID-19 home antigen tests and COVID-19 PCR tests be optimally utilized?
• Is there a role for prophylactic anti-viral therapy and prophylactic use of nutraceuticals?
Who will be at greatest risk for hospitalization and death? There is a spectrum.
When/if potentially more virulent variants arrive, there is a spectrum regarding the extent to which a given infected individual is at risk for severe disease and death:
According to GVB’s analysis, the status of a highly vaccinated individual’s immune system is worrisomely different from the normal immune status of healthy unvaccinated individuals, especially if the vaccinee was vaccinated prior to experiencing productive natural SARS-CoV-2 infection. As stated earlier, the immune system of many vaccinated individuals has needed to do things it normally has not needed to do (e.g., produce high levels of infection-enhancing but virulence-inhibiting PNNAbs and substantial levels of SIR-created broadly neutralizing antibodies) as a result of failing neutralizing antibody capacity; and their cell-based innate immune system has been sidelined and, therefore, unable to adapt to the more infectious environment and hence unable to contribute to herd immunity.
In contrast, the immune system of an unvaccinated individual has increasingly reprogrammed (“trained”) its cell-based innate immune capacity through epigenetic changes to progressively adapt to the increasingly infectious viral landscape. Because their innate immune training compensated for loss of the neutralizing capacity of previously infection-primed antibodies, the unvaccinated did not need to rely on SIR-induced broadly cross-reactive neutralizing antibodies or on virulence-inhibiting PNNAbs to ensure protection from (severe) disease. Whereas unvaccinated individuals develop sterilizing immunity after infection and thereby contribute to herd immunity, COVID-19 vaccination during a pandemic does not result in sterilizing immunity and thereby does not contribute to herd immunity.
Not only has the COVID-19 mass vaccination campaign adversely affected the immune response of the vaccinated individual, but it also collectively altered the immune status of COVID-19-vaccinated populations in that it provoked herd immune selection pressure instead of herd immunity. Indeed, the mass vaccination campaign has been responsible for the natural selection and dominant propagation (or co-circulation) of a continuous succession and vast array of increasingly infectious “immune escape” variants. This vast and increasing array of successively dominant variants would not have occurred in the absence of the mass vaccination campaign.
The virulence-inhibiting effect of vaccinees’ PNNAbs will ultimately become suboptimal and put population-level immune selection pressure on the virus such that a variant that is capable of overcoming that effect will have a competitive advantage, will become naturally selected, and will rapidly propagate. Such new variants will be highly virulent when they infect vaccinated individuals who have been depending on the virulence-inhibiting effect of PNNAbs to prevent severe disease and who otherwise have an adversely altered immune status. In comparison, in the case of healthy unvaccinated individuals, who have trained their cell-based innate immune system to fend off viral infection and have not been relying on virulence-inhibiting PNNAbs, these new emerging variants will not cause severe disease. In other words, a variant that threatens to be “highly virulent” when it infects vaccine-primed individuals will be much less threatening to healthy unvaccinated individuals.
Accordingly, when a “highly virulent” variant arrives (is naturally selected and rapidly propagates in a given community), vaccine-primed individuals will be at greatest risk of severe disease and death, and young healthy unvaccinated individuals will be at least risk. There is no convincing scientific rationale to believe that healthy unvaccinated individuals will be at enhanced risk of severe disease when exposed to such a variant.
The immune system of a highly vaccinated individual—particularly if the individual did not experience productive natural infection prior to vaccination, and also if the individual is elderly, vaccinated with an mRNA vaccine, and already unhealthy with co-morbidities—will have great difficulty meeting the challenge of a highly virulent variant and will need excellent, prompt, and very well-informed medical help and support. Although their COVID-19 vaccination, to date, has provided protection against severe disease and death—thanks largely to the virulence-inhibiting effect of PNNAbs (as well as the other temporarily helpful but unstable, unsustainable, and ultimately harmful immune adjustments mentioned earlier)—this effect will no longer be available to vaccinated individuals once a potentially highly virulent variant arrives, because the virulence of this variant will primarily be due to its ability to overcome the virulence-inhibiting effect of the PNNAbs.
So there is a spectrum regarding the risk of severe disease and death when/if a potentially highly virulent variant appears on the scene. At one end of the spectrum are individuals who have been highly vaccinated (have received an initial series and additional booster doses, with mRNA vaccines), live in highly and rapidly vaccinated countries, were vaccinated prior to experiencing productive natural infection, and are elderly and have co-morbidities.4 At the other end of the spectrum are young healthy unvaccinated individuals who, to date, have had considerable experience with Omicron variants. There is a broad spectrum of risk between these two extremes. People who experienced definite productive SARS-CoV-2 infection prior to receiving COVID-19 vaccination should be much better off than people who were vaccinated prior to ever experiencing natural infection. Natural infection prior to vaccination provides at least some training of the cell-based innate immune system, which, upon subsequent exposure, likely suffices to reduce the viral production rate below the threshold required for triggering immune refocusing and breakthrough infection.
4Note: Healthy vaccinees who only received a single injection of an mRNA-based COVID-19 vaccine or no more than 2 injections with a non-mRNA-based vaccine prior to developing a symptomatic vaccine-breakthrough SARS-CoV-2 infection are thought to have preserved their capacity to train their cell-based innate immune system.
Risk also depends on how “immunologically reactive” a vaccinated person’s immune system was to their vaccination. If their immune system was only minimally (or not at all) reactive to their vaccine dose(s) (i.e., they did not experience a good “take” or “response” to the vaccine), their immune system may not have been primed. Such “non-responders” are not “vaccine-primed” and are, therefore, to be qualified as “unvaccinated.”
There have been concerns (backed by data) that not all “batches” of vaccine have been equal. Some batches might have a greater quantity and/or quality of mRNA than other batches of the “same” product, due to serious quality control issues. As mRNA is prone to degradation, the concentration of intact mRNA in the vaccine may not have been sufficient in many cases where the vaccine was not stored at the recommended freezing temperature or was not immediately injected after thawing; the proportion of non-responders may, therefore, be higher in those who received the Pfizer mRNA vaccine (30 micrograms of mRNA) as compared to those who received the Moderna vaccine (100 micrograms mRNA). As mRNA vaccines trigger SIR in their own right, It is likely that people who have been vaccinated with a non-mRNA vaccine will be better off than those who received mRNA vaccines.
Risk may also depend on the overall state of health of a person. People who are young, physically fit, well-exercised, well-nourished (including having solidly normal Vitamin D levels), emotionally healthy, and do not have co-morbidities may be better equipped to handle a highly virulent variant than elderly individuals who are without these healthy characteristics. And, of course, there is a spectrum of general health status between these two extremes.
How will illness due to a highly virulent variant most likely behave and how will it need to be treated? It largely depends on the immune status of the infected individual.
There is a spectrum regarding how the illness (caused by a highly virulent variant) will unfold in a given individual and how it will need to be treated. It will depend primarily on the vaccination status of the individual (as discussed above) but also on the other general health factors mentioned. Since this represents uncharted territory, it is unknown exactly how the illness will behave and unfold. Below is my best guess. I offer it not with any claim that it is certainly correct, but to stimulate and facilitate proactive scientific dialogue and thoughtful anticipatory planning regarding how illness due to a highly virulent variant might behave and how it might be best monitored, treated, or prevented in the first place.
In the case of highly vaccinated individuals, especially if they did not experience productive natural infection prior to vaccination, we should be prepared for the possibility that the illness will unfold as follows:
Because their immune system will have very little capacity (at either the cell-based innate immunity level or the adaptive immunity level) to control the virus, they will probably quickly become overwhelmingly infected, in the upper respiratory tract (URT), lower respiratory tract (LRT), and possibly other internal organs. They might have very high viral loads in all of these locations. Unfortunately, they will not be able to rely on usual immune mechanisms to control the virus—e.g., NK cells (natural killer cells, which are a key component of the cell-based innate immune system) or on effective utilization of their adaptive immune system. The acute viral phase of their illness may therefore quickly become extraordinarily severe (within 1-3 days) and may last more than the usual 7-10 days. Their immune system may or may not have time, opportunity, or wherewithal to resort to the most primitive, non-specific, and violent of its rapid response mechanisms—-namely, macrophage activation and massive release of cytokines from these macrophages, i.e., desperate production of a massive “cytokine storm.”5,6 But even if the immune system is able to promptly mount a cytokine storm, this desperate effort to protect the person from infection may be too late or may otherwise fail to even partially control the virus—plus, a cytokine storm has great potential to do harm.
In the very worst case scenario the highly vaccinated high risk individual is so unable to immunologically control the highly virulent variant that extremely overwhelming viral infection develops and escalates so rapidly that death occurs before there is time or opportunity for the immune system to even try to mount a potentially protective hyperinflammatory (cytokine storm) reaction. Unfortunately, it is quite possible that this very worst case scenario will be common when highest risk vaccinees encounter a highly virulent variant.
5Note: Although the cell-based innate immune system (e.g., NK cells) in heavily COVID-19 vaccinated individuals is sidelined, cytokine production by the innate immune system is not sidelined.
6Note: For more information about “cytokine storm” and its treatment (both in COVID-19 and in other clinical situations), see the following article: Treatment of Severe COVID-19: https://notesfromthesocialclinic.org/treatment-of-severe-covid-19-illness-long-version/
The best hope for the above-mentioned highly vaccinated high risk patients will be prophylactic anti-viral treatment (initiated well before exposure to the more virulent variant) in an effort to prevent them from developing infection with a highly virulent variant in the first place. (We will return to prophylactic treatment considerations later.) But if such high risk patients do become ill with a virulent variant (either in the absence of prophylactic anti-viral treatment or despite it), their best hope will be prompt initiation of an optimal therapeutic dose of anti-viral therapy as soon after onset of symptoms as possible. However, if that anti-viral therapy is inadequately effective and they have the time, opportunity, and wherewithal to promptly mount a “cytokine storm,” their next best hope is that the cytokine storm will somehow quickly bring the virus under some semblance of control—without the cytokine storm causing severe damage to the patient in the process (or at least before the cytokine storm starts causing severe damage). If both the anti-viral therapy and the cytokine storm (if they are able to mount such a storm) fail to quickly bring the virus under control, the patient will be dependent on prompt, bold, timely, well-informed interventions that are described later in this article—and even those measures may be too little, too late.
To be effective, a cytokine storm would need to be launched by the immune system very early during the course of the overwhelming viral infection, particularly if anti-viral therapy is inadequately effective—-probably within the first 1-3 days after onset of COVID-19 symptoms (as opposed to starting on day 8 or later, which has been the case with severe COVID-19 to date). Instead of a cytokine storm occurring in only a small percentage of patients (which has been the case with COVID-19 to date) and typically occurring only after day 7, a cytokine storm (in those who are able to muster a cytokine storm) will likely occur in a high percentage of high risk patients and will likely occur 1-3 days after onset of symptoms. In other words highly vaccinated high risk patients (those who survive the overwhelming viral assault on the first 1-3 days) will end up in the ICU within the first week of their illness rather than during the second or third week, and a higher percentage of them will end up in the ICU.
There is a fine line between the cytokine storm being helpful and being harmful. It is a double-edged sword. Although the cytokine storm might initially help control the virus infection, the cytokine storm will quickly become organ-threatening and life-threatening because of the massive inflammation and harmful cascading problems it can create.
This combination of overwhelming viral infection and massive cytokine storm (if the patient has time and is able to muster such), occurring in rapid succession (even simultaneously) early in the course of the illness (during the first week, even early during that week) creates a difficult therapeutic dilemma for the hospitalists or ICU physicians. On the one hand, the patient is suffering from overwhelming viral infection (with a high viral load); on the other hand, the patient is experiencing a potentially life-threatening cytokine storm that may or may not be able to reduce the viral load. Complicating matters is the fact that the anti-viral therapy that should be administered as early as possible, may or may not be adequately effective.
Under the above circumstances, the physician will need to quickly and serially estimate the patient’s viral load (at a given point in time and serially thereafter), quickly determine whether (and to what extent) the patient (at that same moment in time) is experiencing a cytokine storm, and decide whether that cytokine storm is doing more harm than good (or vice versa). In addition to providing anti-viral treatment, the physician will need to decide whether and when to protect the patient from life-threatening damage potentially (and likely) wrought by the cytokine storm. Ideally, this decision should be informed by promptly, prospectively and serially collected clinical data (on the given patient) regarding the extent to which the anti-viral therapy and/or cytokine storm have reduced the viral load (not just in the URT but also in the LRT) and the extent to which the cytokine storm is beginning to cause more harm than good. The best available way to estimate the viral load would be to prospectively follow serial PCR tests (paying close attention to the Ct values at which tests are positive), initially in the URT, but soon (if indicated and if the benefits are perceived to outweigh the risks) in the LRT (by swabbing bronchial mucosa). (See discussion of Ct values later.) The best way to serially monitor the intensity and course of the cytokine storm and the threat it is posing is to serially follow serum ferritin levels, CBC, ESR, CRP, liver function tests, d-Dimer, etc. Serial serum ferritin levels are particularly helpful. We would like to see initially high ferritin levels substantially and quickly falling towards the normal range.
The temptation on the part of the physician will be to withhold immunosuppressive treatment of a harmful cytokine storm out of concern that such treatment might interfere with the potential anti-viral effect of the anti-viral medication and/or the anti-viral effect of the cytokine storm. However, if treatment of the cytokine storm (with high dose corticosteroid and anti-cytokine therapy, such as anakinra or tocilizumab) is delayed for too long, the risk of severe organ damage and death from cytokine storm, with or without concomitant overwhelming viral load, rapidly increases.
It may prove best to give anti-viral treatment and initial cytokine storm at least a brief chance to at least partially control the virus, but be prepared to quickly shift to prioritizing anti-cytokine storm therapy as soon as an adequate decrease in viral load has occurred or as soon as it becomes apparent that the cytokine storm can no longer be left inadequately treated. This will be a difficult and uncomfortable decision. In an individual patient the relative risk of effectively treating cytokine storm versus the risk of not adequately treating cytokine storm is difficult to discern and may be equal. Serial testing of viral load (in the URT and, if indicated, in the LRT) and serial monitoring of the cytokine storm will be helpful and critically important. Careful and frequent monitoring and repeated re-evaluation of the patient will be essential. A balanced, titrating approach, based on frequent reassessments will be key. It will be necessary to be both appropriately bold and appropriately cautious. Timing will also be extremely important—initiating therapies neither too soon nor too late. The “Art” of medicine, as well as the science of medicine, will need to be optimally practiced. It may not be possible to save some patients, even with best possible decision-making.
Bear in mind that it is quite possible that the cytokine storm triggered by the highly virulent variant in high risk highly vaccinated individuals (if they have time, opportunity, and the wherewithal to mount such a storm) will be more massive and explosive than has ever been seen in many adult ICUs. The cytokine storm might require extraordinarily high doses of anakinra,7 e.g., and a very large number of patients might need such treatment. Pulses of high dose IV methylprednisolone may also be needed. Accordingly, an important anticipatory step (to be taken now) would be to ramp up global production of anakinra (as well as tocilizumab and IV methylprednisolone) so that all patients who need these medications will have prompt access to them.
7Note: Regarding anti-cytokine therapy for severe cytokine storm, my personal preference is anakinra, rather than tocilizumab. Anakinra has a more rapid onset of action, a much shorter half-life, and a much broader range of safe dosage. The dosage of anakinra can be quickly titrated upwards, as needed, and steadily titrated downward as the patient improves. Anakinra is far more flexible than tocilizumab.
It is highly likely that current global supplies of anakinra and tocilizumab are woefully inadequate to meet the need that may occur when a highly virulent variant arrives. It would be a shame if the supply of these medications falls short of the need for them. Also, to date (i.e., historically), the prices charged for anakinra and tocilizumab have been exorbitant. It would be a shame if the price for anakinra and tocilizumab results in these medications being unaffordable for treatment of cytokine storm triggered by a highly virulent variant. Production of anakinra and tocilizumab, therefore, needs to be immediately and greatly ramped up (at “warp speed”) and the price of these medications needs to be immediately ramped down!!
Patients who present with severe SARS-CoV-2 infection and severe cytokine storm (as described above) may also benefit from prompt administration of high dose IV (intravenous) Vitamin C and thiamine and may need prompt treatment with heparin. (See the MATH+ protocol that is detailed on the excellent FLCCC website: www.covid19criticalcare.com
Management of most healthy unvaccinated patients will likely be much less difficult. They will be better able to handle the highly virulent variant and will be less likely to develop cytokine storm. Although the “highly virulent variant” will, indeed, be highly virulent in high risk heavily vaccinated individuals (because the immune status of heavily vaccinated individuals has been altered by the mass vaccination campaign and they have been depending on virulence-inhibiting PNNAbs, which the highly virulent variant is able to overcome), the “highly virulent variant” will not be as virulent in healthy unvaccinated individuals (because their immune systems will be intact and able to respond in a normal way, and they have not been depending on virulence-inhibiting PNNAbs). As explained earlier, the immune status of heavily vaccinated individuals has become abnormal and is now quite different from the normal immune status of healthy unvaccinated individuals.
When the highly virulent variant arrives, it is appropriate to believe that the illness it will cause in healthy unvaccinated individuals will, at worst, resemble the mild-moderate cases of COVID-19 that were typical during the first 3.5 years of the pandemic. But there is no guarantee that unvaccinated individuals (particularly those who are elderly and/or have co-morbidities) will experience only mild-moderate illness. We need to be prepared for the possibility that some unvaccinated individuals, particularly elderly individuals with co-morbidities, may become severely ill and may need the same prompt, excellent, well-informed clinical care that highly vaccinated individuals may need.
In between the two above-described extremes—at one extreme, a rapid life-taking course in the high-risk highly vaccinated (without time, opportunity, or wherewithal to even mount a potentially helpful cytokine storm) and, at the other extreme, a far less severe course in the healthy unvaccinated—will be a spectrum of courses, with varying degrees and rapidity of viral clearance, varying incidence of cytokine storm, varying degrees (and timing) of cytokine storm, varying effectiveness of cytokine storm, and varying damage from cytokine storm. Monitoring and treatment will need to be patient-specific—i.e., individualized, according to a patient’s position along the spectra discussed above.
Is there a role for prophylactic anti-viral therapy?
Given the worrisome way in which illness due to a highly virulent variant is likely to behave, at least in the highest-risk highly vaccinated, is there a role for prophylactic anti-viral therapy?
It seems appropriate to strongly consider prophylactic anti-viral therapy,8,9 at the very least for people who are at particularly high risk of developing life-threatening illness when they contract the highly virulent variant. Prophylactic anti-viral therapy should be strongly considered for health care workers, including staff in retirement homes and nursing homes, to protect those workers and the people they serve. Prophylactic anti-viral therapy would be least important for young healthy unvaccinated individuals. However, in populations where the highly virulent variant is widely circulating (or threatens to widely circulate), one could build a very strong case for encouraging prophylactic anti-viral treatment for virtually all people, including those who are healthy and unvaccinated—for the sake of protecting high risk patients. Such widespread prophylactic anti-viral therapy could substantially reduce the quantity of virus circulating in the population as a whole and, thereby, reduce likelihood of infection of the most vulnerable. In other words, young healthy unvaccinated individuals would not necessarily need or want to take prophylactic anti-viral medication for their own sakes, but they may choose to take prophylactic anti-viral medication in an effort to help protect the most vulnerable—particularly since we do not have herd immunity.
In addition to prophylactic use of anti-viral therapy, an important component of prophylactic protection is regular use of nutraceuticals to establish and maintain optimal levels of Vitamin D, Zinc, Vitamin C, etc.
8Note: For purposes of this discussion, “anti-viral therapy” refers to therapies such as nirmatrelvir/ritonavir (Paxlovid), remdesivir, molnupiravir, ivermectin, and hydroxychloroquine—and not to nutraceuticals (vitamin D, Zinc, etc.)
9Note: Although the safety of prolonged prophylactic use of hydroxychloroquine has been well-established (e.g., for malaria and for control of lupus) and there has been considerable (and favorable) experience with prolonged prophylactic use of ivermectin for protection against COVID-19, there is no experience with prolonged (or even short term) prophylactic use of Paxlovid, remdesivir, or molnupiravir, regarding safety or efficacy, and, therefore, prophylactic use of Paxlovid, remdesivir, or molnupiravir cannot be recommended.
What are the indications for early introduction of anti-viral therapy during acute illness due to a highly virulent variant of SAARS-CoV-2?
Those who are at high risk for severe disease when infected with a highly virulent variant (e.g. the highly vaccinated who were vaccinated prior to experiencing productive natural infection and those with co-morbidities) should be started on an optimally therapeutic dose of anti-viral therapy as early as possible when/if they develop acute illness—e.g. on day one, ideally. Early introduction of anti-viral therapy should also be strongly considered for healthy unvaccinated individuals when they become ill with COVID-19, particularly if the person is elderly and/or has co-morbidities. Early introduction of anti-viral therapy for virtually all people infected with the highly virulent variant might be strongly considered for one other important reason—-as a way to reduce the overall viral load in a hospital and community and thereby protect hospital workers, nursing home care givers, and the most vulnerable members of a community. In a community that is experiencing a great amount of circulating virus, treatment of all citizens (except for children?), regardless of whether they are ill, with a therapeutic dose of anti-viral therapy (for approximately 2 weeks or longer?) might be a consideration—in an effort to eradicate the virus from the community (or at least substantially reduce the amount of virus circulating in the community), again for the sake of protecting the most vulnerable—particularly since we do not have herd immunity.
What anti-viral therapy has the most favorable benefit/risk ratio?
The best way to have determined which of the available anti-viral therapies has the most favorable benefit/risk ratio would have been to conduct a large, careful, high-quality, objective, honest, head-to-head study that compares all available anti-viral therapies for SARS-CoV-2—-for example, a comparison between Paxlovid, remdesivir, molnupiravir, ivermectin (IVM), and ivermectin plus hydroxychloroquine (HCQ). Unfortunately, despite the fact that we are nearing the end of the 4th year of the pandemic, and despite the obvious need for such a comparative study, no such study has been conducted. So, we do not have optimal comparative data regarding which of those five treatment options has the most favorable benefit/risk ratio.
When issues of conflict of interest, quality of data collection, honesty of data analysis, honesty of data presentation, quality and quantity of safety studies, issues of publication integrity, drug cost, and actual clinical and public health experience on the frontlines (e.g., in Mexico City, Uttar Pradesh, Peru, and Honduras) are taken into account, the anti-viral medication that appears, by far, to be most trustworthy and appears, by far, to have the most favorable benefit/risk ratio is not Pfizer’s Paxlovid or Merck’s molnupiravir or Gilead’s remdesivir, but ivermectin or the combination of IVM and HCQ.
In my opinion, IVM or IVM plus HCQ are the best options and have the most favorable benefit/risk ratio. Personally, I am greatly impressed by the experiences that physicians in Honduras, Mexico City, Peru, Uttar Pradesh, and many other countries have documented with the Nobel prize-winning drug, ivermectin, which is a unique and truly extraordinary drug that has saved millions of people from the devastation of river blindness and elephantiasis. Meta-analysis, controlled clinical studies (including at least 21 randomized controlled studies), observational studies, and the published experiences of many public health departments with widespread anticipatory use of IVM—have provided compelling scientific evidence that IVM is the anti-viral drug of choice for the prophylaxis and treatment of COVID-19. Personally, I have been absolutely appalled by the unscientific, corrupt, and unethical ways in which promoters of the mass vaccination campaign have demonized ivermectin, ignored studies that have documented its efficacy, produced fraudulent counter-studies, and have censored, belittled, ridiculed, and punished physicians for advocating treatment of COVID-19 with ivermectin. There is no place for such behavior in science, medicine, or public health. (Please see Dr. Pierre Kory’s excellent and trustworthy book about ivermectin, The War On Ivermectin. It is a must read.)
Unfortunately, head-to-head comparative studies have not been done. If they were to be done, they would need to be performed according to the strictest of scientific and ethical principles. Sadly, during the COVID-19 pandemic, those fundamental principles have not been adequately practiced by the promoters of the prevailing COVID-19 narrative, as I have explained in several other writings—see: https://notesfromthesocialclinic.org/how-would-three-of-canadas-greatest-historical-figures-respond-to-the-covid-situation-if-they-were-alive-today Unfortunately, pharmaceutical companies have had grossly inappropriate influence and control over data collection, data analysis and the reporting of data.
For more information on scientific studies and recommendations regarding ivermectin and hydroxychloroquine, as well as the role of nutraceuticals and other treatments of COVID-19, the reader is strongly encouraged to access the following excellent websites and other sources of information:
• FLCCC website: www.covid19criticalcare.com
• Canadian COVID Care Alliance website: https://www.canadiancovidcarealliance.org/
• McCullough Protocol: https://www.amjmed.com/article/S0002-9343(20)30673-2/fulltext
• Dr. Pierre Kory’s book, The War On Ivermectin.
• Interview of South African physician, Dr. Shankara Chetty, by Dr. Philip McMillan: https://www.youtube.com/watch?v=Nj8kOxAcUos
• Interview with Honduran physician, Dr. Fernando Valerio, by Dr. Philip McMillan:
o https://streamyard.com/4q9fgua5cvem
o https://philipmcmillan.substack.com/p/why-was-the-covid-success-from-honduras?utm_source=substack&utm_medium=email&utm_campaign=email-half-post&r=10zdde#play
What is the role of anti-thrombotic treatment of COVID-19?
Abnormal clotting (microvascular thrombosis as well as macrovascular thrombosis) can complicate COVID-19. This potential complication needs to be kept in mind throughout the course of the illness, because it can start developing early (during the first week), though it may not become manifest until later. Prospective, serial monitoring for thrombosis is, therefore, essential, starting with d-Dimer and platelet counts. Early treatment with aspirin (for its beneficial anti-platelet effect) may be appropriate. Early treatment with an oral anticoagulant (e.g. apixaban) might be indicated in some patients, including outpatients. Early treatment with heparin may be appropriate, especially for high-risk highly vaccinated inpatients.
What other early treatments should be considered?
In addition to the already-mentioned treatments, several other “early treatments” can be considered for patients as soon as they become ill with COVID-19. Nutraceuticals (most importantly, Vitamin D, Zinc, Vitamin C, and Thiamine) are particularly important. Nasal sprays (with diluted povidone iodine) and mouth washes (e.g., with Scope) can be quite helpful. Azithromycin, famotidine, and fluvoxamine are options. In some patients early treatment with promethazine (at the onset of suspected pulmonary disease) may be appropriate. Montelukast may be a consideration in some patients. Antibiotic coverage for possible secondary bacterial infection of the LRT may also be needed.
Please see the excellent websites mentioned above for specific details.
For inpatients please note the important roles for intravenous Vitamin C and thiamine (part of the MATH+ protocol), as explained in the excellent FLCCC protocol for hospitalized patients.
The role of pulse oximetry monitoring:
When a highly vaccinated individual who is at particularly high risk of developing severe disease when infected by a highly virulent variant (e.g., elderly individuals with co-morbidities who were vaccinated prior to any productive natural infection) develops COVID-19, it would be wise to frequently use pulse oximetry to monitor the oxygen saturation in their blood. Pulse oximeters can be purchased in drug stores and used in one’s home. If an outpatient serially monitors their oxygen saturation with a pulse oximeter, starting soon after onset of symptoms, and the results remain stable in the normal range, this can be reassuring. If, however, serial monitoring reveals that oxygen saturation is dropping below the normal level, this would be cause for concern. Serial monitoring of oxygen saturation can greatly improve early detection of when/if a patient is developing potentially worrisome pulmonary disease—due either to severe viral infection in the LRT, or severe cytokine storm that is causing severe inflammation in the LRT, or micro or macro thrombosis within the lungs, or secondary bacterial infection in the LRT, or various combinations of these problems. People who are at less risk for severe disease may also want to monitor their oxygen saturation, primarily for reassurance.
Regarding COVID-19 PCR testing:
The COVID-19 PCR tests10 have usually been used to provide only a “positive” or “negative” result, not a quantitative result. If the test is positive, the extent to which it is positive (strongly, weakly, or in-between?) has not routinely been reported to the physician or patient. Although the COVID PCR tests were not specifically designed to indicate the quantity of virus present (viral load), they can be used to provide a rough estimate of the viral load—by paying attention to the Ct (cycle threshold) value at which a test became positive.
10Note: For detailed information about the COVID-19 PCR test, see the following article: The Importance of Knowing the Ct Value at which a COVID PCR Test is Positive: https://notesfromthesocialclinic.org/the-importance-of-knowing-the-ct-value-at-which-covid-pcr-tests-are-positive-long-version/
When a COVID-19 PCR test is positive, the Ct value represents the number of times the molecular material in the specimen needed to be amplified before it was possible for the testing machine to detect the presence of fragments of the SARS-CoV-2 virus. If only 10 cycles of amplification were needed, that would mean that there was an enormous amount of SARS-CoV-2 viral material in the specimen. If 20 cycles of amplification were needed, that would suggest that a large amount of SARS-CoV-2 viral material was present, but not an enormous amount. If 28 cycles of amplification were needed, that would correlate with presence of a relatively small-moderate amount of the virus. If more than 32 cycles of amplification were needed to detect presence of possible SARS-CoV-2 viral material, the result, although “positive,” is not reliably interpretable—it may or may not mean that SARS-CoV-2 viral material is truly present, and even if the detected material is truly SARS-CoV-2 material, it could simply mean that a few fragments of dead virus were present. If the test does not become positive until 40, 45, or 50 cycles of amplification have been performed, such a “positive” result is inadequately interpretable, totally unreliable, and certainly could represent a “false positive.”
Unfortunately, most of the laboratories (at least in the USA) initially programmed their PCR testing equipment to stop looking for SARS-CoV-2 viral material only after at least 40 cycles of amplification had been performed. In other words, the test result was reported as negative only if the test was still negative after 40 cycles of amplification. Some labs have set their equipment to continue amplifying until 45 (or 50) cycles of amplification have been completed—a practice that surely generates many false positives.
If a COVID-19 PCR test is “positive,” it is important and helpful to know whether it was positive after only 10 cycles of amplification (i.e., at a Ct value of 10) or only after 40 cycles of amplification (at a Ct value of 40), or at a Ct value somewhere in-between (e.g., at a Ct value of 15, 20, or 25). Such information would provide at least a rough, but valuable, estimate of the viral load.
For example, if all residents in a nursing home were to undergo COVID-19 PCR testing and 20% of them were found to have a “positive” test, it would be important to know whether all of those positive tests were positive at a Ct value less than 28, or all of the positive results were positive only after 40 cycles of amplification (at a Ct value of 40). The latter result would not necessarily mean that any of those “COVID-19 positive” patients truly had COVID-19.
Likewise, if an asymptomatic professional basketball or football player tests “positive” before an important game, it would be important to know whether the “positive” test was positive at a Ct of 10 or 45. The latter result would be totally unreliable.
The above discussion points out how important it is to know the Ct value at which any “positive” PCR test had become positive.
The above discussion also reveals the value of serially following COVID-19 PCR results in a given patient (with disclosure of the Ct value of all positive tests). If, for example, a patient initially had a positive PCR test at a Ct of 10 (meaning that the patient was carrying a huge load of virus at that time), but two days later had a positive test at a Ct of 18, then 2 days after that the test was positive only at a Ct of 24, then 2 days after that the test was positive only after 35 cycles of amplification (meaning that there was little, if any live virus still present in the specimen, possibly just dead fragments, if that)—this would suggest that the patient was clearing the virus very well. On the other hand, if a given patient’s serial PCR tests are all positive at a Ct in the range of 16 and are showing no signs of improving, that would suggest that the patient is having difficulty clearing the virus.
What if a patient is on day 8 (or earlier) of their illness and suddenly becomes much more severely ill? Are they worsening because the virus is surging and overwhelming them? Or are they worsening, instead, because their immune system has accelerated into a harmful hyperinflammatory phase that is making them severely ill, despite clearance of the virus (or substantial reduction of the viral load)? Or, are both problems occurring? If both problems are occurring, which is the more threatening problem? In such a circumstance it would be helpful to know whether the patient’s PCR test was still positive, and if so, at what Ct value. As discussed below, in such a circumstance it is important to realize that the result of a PCR test on a nasal swab may or may not be the same as the result of a PCR test done on a swab from the lower respiratory tract (LRT).
COVID-19 PCR test results on a swab from the lower respiratory tract (LRT) versus a swab from the nasal passages:
The result of a PCR test on a nasal swab (with close attention paid to the Ct value at which the test is positive) may or may not be the same as the result of a PCR test (and Ct value) performed, simultaneously, on a swab (if clinically indicated and if the benefit of obtaining such a sample is perceived to outweigh the risk) from the lower respiratory tract (obtained, e.g., upon bronchoscopy or when a patient is intubated). For example, conceivably, a patient in the hospital could have a strongly positive PCR test (i.e., a positive result at a low Ct value) on a nasal swab (due to a high viral load in their nasal passages) but a negative PCR test (if clinically indicated and performed) on a simultaneously obtained swab of their bronchial mucosa (because their immune system was able to prevent or control infection of their LRT). Another patient, one in the ICU, might have equally positive PCR test results (i.e. equal Ct values) in the nasal passages and the LRT, due to equally severe infection in both locations. It is also conceivable that a patient in the ICU could have a negative (or minimally positive) PCR test in their nasal passages (because their immune system was able to clear the virus in that location) but a strongly positive PCR test in the LRT (because of great difficulty clearing severe infection in the LRT). Therefore, in a hospitalized patient, it may not be correct to assume that the result of a PCR test on a swab of the bronchial mucosa (if clinically indicated) would be the same as a simultaneously obtained swab of the nasal mucosa.
If a patient has a negative (or minimally positive) PCR result on a nasal swab and does not have evidence of LRT disease (no LRT symptoms or radiographic evidence of pneumonia), then it is reasonable to assume that a PCR test on bronchial mucosa (if it were to be done) would also be negative or minimally positive, and, therefore, would not need to be done. If a hospitalized patient with COVID-19 has a negative or minimally positive PCR test on a nasal swab performed on day 8, for example, of their illness (or earlier) but has evidence of considerable LRT disease, it is important to ask: Is the LRT disease due to active viral infection in the LRT; or is it due to a great amount of inflammatory immune reaction in the LRT without significant accompanying ongoing active viral infection; or is it due to a combination of active viral infection and an intense inflammatory immune reaction (and if so, which component is most threatening). Most likely, such a patient’s most threatening problem in the LRT is intense immune-mediated inflammation. To answer this question with greater certainty, it would be helpful to know whether a COVID PCR test on a swab from the bronchial mucosa is positive and, if positive, to know the Ct value at which it was positive.
Whether the benefits of performing such a test on a particular patient outweigh the risks is a matter of clinical judgment. Whether PCR results on a bronchial swab are needed (for a given patient) is also a matter of individualized clinical judgment. Some experienced physicians may feel comfortable concluding that such a patient’s most threatening problem is immune-mediated inflammation (not ongoing viral infection), and they may feel comfortable proceeding with appropriately aggressive immunosuppressive treatment (e.g. appropriately high doses of methylprednisolone and anakinra) without obtaining a COVID-19 PCR test on a bronchial swab. Other physicians may feel very hesitant (even unwilling) to initiate appropriately aggressive immunosuppression in this context without first documenting the results of a PCR test on bronchial mucosa. If a patient who needs immunosuppressive therapy will not receive it unless the results of a PCR test on a bronchial swab convince the physician that it is appropriate to give such immunosuppression, then the benefits of doing the test might outweigh the risks.
In addition, tests can be done to gauge the extent of inflammation/cytokine storm. If a PCR test on bronchial mucosa (if done) is negative, and tests for cytokine storm are positive, this would provide strong support for the notion that the considerable inflammation in the LRT is not due to active viral infection in the LRT but, rather, to an intense inflammatory immune reaction that has successfully cleared the virus but has left the LRT severely inflamed—in which case immunosuppression would be appropriate.
Why have Ct values not routinely been included in the official lab reports of positive COVID-19 PCR tests?
It is unclear why Ct values have not routinely been included in the official lab reports of all positive COVID-19 PCR tests. In many hospitals and clinics the Ct values of “positive” tests have not been routinely disclosed to patients or their physicians. Many physicians have never heard of the Ct value and, therefore, do not even know to ask for it.
One explanation for the policy of not disclosing Ct values has been the claim that “including the Ct value in the PCR report would create too much confusion. It would take too much time for lab personnel to explain a reported Ct value to an inquiring physician, and it would take too much time for physicians to explain Ct results to their patients. Besides, there is considerable variability in Ct results, depending on the manufacturer of the PCR test and on the correctness and uniformity of lab technique. When a swab from the same person is tested with two different test kits, or in two different labs, the two Ct values might differ. This could lead to confusion and false conclusions. It would open up a huge can of worms to disclose Ct values.”
There is some truth to the above claims. However, despite the above complexities and limitations, patients and their physicians deserve to know and need to know the Ct value of any positive test. Whatever amount of time and effort is needed to educate physicians and patients about a Ct result should be spent. And laboratory regulatory bodies can and should ensure that there is better uniformity of Ct results among different manufacturers and in different labs. There is no legitimate scientific, clinical, or ethical excuse for not disclosing the Ct value of all positive tests and for not thoroughly educating physicians, patients, and the general public about Ct values.
Regarding home antigen testing for COVID-19:
In anticipation of a highly virulent variant, it will be important for outpatients with COVID-19 to do home COVID-19 antigen tests early (within 1-2 days after onset of symptoms) and serially (every 1-3 days, as needed).
The home antigen tests provide a “positive” or “negative” result, regarding presence or absence of SARS-CoV-2 antigen (nucleocapsid) in the nasal mucosa. Although the home antigen tests were not specifically designed to indicate the quantity of virus present (viral load) and have not been formally tested to determine whether they can be used to estimate viral load, I would like to share observations that suggest that serial home antigen testing might provide some helpful information regarding initial and subsequent viral load.
At the very beginning of COVID-19 illness (during the first 24 hours after onset of symptoms) it is possible that the home antigen test will be negative. That is, after about a minute, the “Control” bar becomes brightly positive, but the “Test” bar remains unequivocally negative throughout the entire 15 minutes of the test.
At some point within the first two days of illness, the home antigen test is apt to become positive. In some such instances, the test quickly becomes very strongly positive—e.g., the “Test” bar might become very bright even before the “Control” bar becomes similarly bright.11 In other instances, the “Control” bar becomes very bright (as usual) at the usual one minute mark (or so) and the “Test” bar becomes only faintly positive at about the same time (even later) and becomes only a little brighter during the remaining minutes of the test. A spectrum of possibilities is possible between these two extremes.
It is tempting to think that in the first instance the rapid onset of a brightly positive “Test” bar (even before the “Control” bar becomes positive) means that a very high viral load is present; and that in the second instance the delayed appearance of only a faintly bright “Test” bar means that the person has only a low load of virus. This is assuming that in both instances the nasal swabbing and use of the test kit were done correctly and equally correctly. Although it is tempting to conclude such, it is wise to not draw that conclusion with any certainty. But, with each testing, it is worth noting and recording how strongly positive the “Test” bar became and how soon it reached its maximum brightness (positivity).
If an individual person’s initial test (during the first 1-2 days after onset of symptoms) was strongly positive (e.g., the “Test” bar became very strongly positive even before the “Control” bar turned positive) and then, upon serial testing (repeat testing every 1-3 days), the “Test” bar became positive increasingly less quickly and increasingly less brightly and eventually became negative (on day 8-10, e.g.), it is tempting to think that those particular serial test results indicate that the person’s viral load was substantially, steadily, and increasingly diminishing and that little or no virus was still present by day 8-10. Again, although it is tempting to conclude such, it is wise to not draw that conclusion with any certainty. But it is worth noting, recording, and comparing how strongly positive the “Test” bar became and how soon it reached its maximum brightness (positivity) on each of the serial tests.
Again, the COVID-19 home antigen tests were not designed for quantitation of viral load, nor have they been tested to determine whether they can be reliably used in the above fashion to grossly estimate (and serially follow) viral load. But, paying attention to such details, initially and serially, seems better than ignoring such details, as long as the limitations of doing so are kept in mind.
It is unclear why formal studies have not been done to determine the extent to which serial home antigen tests can be reliably used in the above-described fashion to serially estimate viral load. Common sense suggests that it would have been important and helpful to have conducted such a study, long ago.
11Note: It is important to realize that a very strongly positive COVID-19 PCR or home antigen result does not necessarily mean that severe disease is imminent or likely. What matters most is the extent to which a person’s immune system is able to efficiently handle a particular viral load. If a person’s immune system is healthy, it can efficiently manage even a very high viral load and the result can be relatively mild or moderate disease.
CLOSING COMMENTS:
Notice that I have not mentioned booster doses of “updated” vaccine as an appropriate proactive response to the potential (and highly likely) surge of a highly virulent variant. As explained in other articles, the COVID-19 mass vaccination campaign has been the cause of the extremely difficult situation we are now facing. It is not the solution. We would not now need to think about and prepare for the tragic clinical scenarios described in this article, if the COVID-19 mass vaccination campaign had never been implemented. In my view, the COVID-19 vaccines should be immediately withdrawn from the market.
Of all the proactive interventions mentioned in this article (in anticipation of a highly virulent variant), mass anti-viral therapy with ivermectin makes the most sense. Mass prophylaxis with ivermectin could protect individuals and communities by preventing or minimizing the amount of a highly virulent variant that gains a foothold and circulates in their community. Once a highly virulent variant does gain a foothold in a community and begins to circulate widely and cause illness in that community, mass treatment of the community with a therapeutic dose of ivermectin (as opposed to a lower and/or less frequent prophylactic dose) for at least two weeks might largely eradicate the virus from that community, thereby protecting the most vulnerable.
By using ivermectin in the above manner, it is quite possible that a huge number of hospitalizations and deaths could be prevented. We should learn from places like Uttar Pradesh. Such an approach would also be the least expensive approach, by far, and could be implemented equitably throughout the world.
At the very least, it is hoped that this article will stimulate and facilitate respectful scientific dialogue among physicians, nurses, other health care workers, public health officials, and the general public regarding how to best prepare for the potential arrival of a highly virulent SARS-CoV-2 variant.
RELATED READINGS:
For additional thoughts and suggestions regarding how to prepare for and meet the challenge of a highly virulent variant, please see the original article, In Anticipation of a Highly Virulent SARS-CoV-2 Variant: https://notesfromthesocialclinic.org/in-anticipation-of-a-highly-virulent-sars-cov-2-variant/
Also, please see: How Has the COVID-19 Mass Vaccination Campaign Made the Natural Selection and Rapid Propagation of a Highly Virulent Variant Highly Likely? https://www.trialsitenews.com/a/how-has-the-covid-19-mass-vaccination-campaign-made-the-natural-selection-and-rapid-propagation-of-a-highly-virulent-variant-highly-likely-44952cc7
For additional information, see the many articles that are posted in the “Notes on COVID-19” section of the following website: www.notesfromthesocialclinic.org
In particular, please see the following articles:
Respecting the Immune Ecosystem: https://notesfromthesocialclinic.org/respecting-the-immune-ecosystem-slide-by-slide-written-transcript/
Treatment of Severe COVID-19: https://notesfromthesocialclinic.org/treatment-of-severe-covid-19-illness-long-version/
The Importance of Knowing the Ct Value at which a COVID PCR Test is Positive: https://notesfromthesocialclinic.org/the-importance-of-knowing-the-ct-value-at-which-covid-pcr-tests-are-positive-long-version/
How Would Three of Canada’s Greatest Historical Figures Respond to the COVID Situation If They Were Alive Today? https://notesfromthesocialclinic.org/how-would-three-of-canadas-greatest-historical-figures-respond-to-the-covid-situation-if-they-were-alive-today
An Open Letter to Parents and Pediatricians https://notesfromthesocialclinic.org/an-open-letter-to-parents-and-pediatricians-2/
Also, please see articles posted on Dr. Geert Vanden Bossche’s website: www.voiceforscienceandsolidarity.org
And, read Dr. Vanden Bossche’s recent book, The inescapable Immune Escape Pandemic.
DISCLAIMER:
The information in this article is intended for educational and discussion purposes only and should in no way replace the ongoing medical advice of your own health care provider.
The information in this article is not intended as a substitute for consultation with a licensed healthcare practitioner, such as your physician.
Before you make any changes in your health care decisions or plans, please consult your physician or another licensed healthcare practitioner to thoroughly discuss relevant information—including (only if you wish) statements, understandings, explanations, opinions, suggestions, and recommendations provided in the writings on this website. Your health care provider knows you and your medical history best. My hope is that you have a good relationship with your health care provider such that you can have a mutually respectful discussion about what treatments and recommendations are best for you.

Rob Rennebohm, MD